MRI-TRUS Fusion
How do we diagnose prostate cancer?
For many years, the standard method of diagnosing prostate cancer was fairly crude. The first step required a primary care physician to perform a digital rectal exam and prostate specific antigen (PSA) test on the patient. If a nodule was detected, or if PSA was greater than 4, the patient was referred to an urologist. A transrectal ultrasound-guided (TRUS) biopsy was performed by the urologist; 8 to 12 needles were inserted into the prostate gland in a relatively blind fashion.
There was no real attempt to identify a specific tumor or suspicious target. Ultrasound images were used only to ensure samples were acquired safely from various regions of the prostate gland. While this method is responsible for many diagnoses of prostate cancer, it subjected many men to unnecessary harm and resulted in increased costs.
In some instances, TRUS was performed in response to elevated PSA caused by an enlarged gland, not prostate cancer, when PSA density was not calculated to normalize PSA levels. In other instances, TRUS biopsy resulted in the misclassification of prostate cancer aggressiveness according to the Gleason score. This can lead to inappropriate treatment recommendations based on inaccurate data. Some men also experienced complications from the procedure, such as infection (prostatis) and rectal bleeding.
If an initial TRUS biopsy did not detect cancer, and the patient’s PSA remained elevated, he was instructed to return in one year for another TRUS biopsy. This process was repeated either until a cancer grew large enough to be sampled by ‘chance of the needle’ or until a frustrated patient refused to continue repeat TRUS biopsies. Neither of these scenarios is acceptable.
Fortunately, developments in MRI technology now allow physicians the ability to better visualize the prostate and detect cancer.
How can we improve prostate cancer detection?
Ultrasound is generally too insensitive to allow for tumor nodule detection. It is also poor at separating benign nodules in the prostate’s transition zone from a tumor. However, there have been major developments in prostate imaging since 2007.
Several major academic centers in the Netherlands, France and the United States have improved specific MRI imaging protocols to advance optimal imaging of the prostate gland.
Early research demonstrates how MRI can detect prostate cancer using functional imaging sequences and high field strength 3 Tesla (3T) MRI machines. Functional data is collected during:
- Dynamic contrast-enhanced (DCE) imaging.
- Diffusion weighted imaging (DWI).
- MR spectroscopy.
Prostate MRI Functional Imaging Sequences
In DCE images, prostate tumors enhance earlier in time than normal tissue, show a higher peak enhancement than normal tissue and wash out contrast more quickly than normal tissue. This allows post-processing software to generate a time function curve that improves tumor node visualization. This technique is especially effective at detecting tumors in the peripheral zone where 65 percent of tumors are located.
DWI is especially effective at detecting tumors in the transitional zone and central zone. Aggressive tumor cells tend to be more tightly packed together than healthy cells or slow-growing cancer cells, which restricts free water motion within the tumor nodule. Using DWI, experienced radiologists can measure cell density and determine the tumor’s apparent diffusion coefficient (ADC).
MR spectroscopy reveals metabolic differences in prostate tissue that can indicate cancer. Because prostate cancer is associated with lower levels of citrate and higher levels of choline and creatine, this technique is especially useful for tumor volume detection and cancer staging.
High quality anatomic imaging with 3T magnets also allows radiologists to score each region of the gland by incorporating the functional data. This scorecard allows a stratification of risk and aggressiveness. This information allows radiologists to perform targeted biopsy in bore using real-time MRI guidance, with the goal of sampling the most aggressive elements of suspicious tumor nodules.
Benefits of Prostate MRI
Data from multiple early implementers of prostate MRI have explored the efficacy of prostate MRI and subsequent MRI-guided biopsy.
They found that the specificity and sensitivity for finding clinically significant prostate cancer (those with a Gleason score of 6 or higher and a volume exceeding 5 millimeters) was between 85 percent and 96 percent. Their data also show a negative predictive value around 95 percent, which means there was a 95 percent chance that no significant prostate tumor existed if prostate MRI did not identify a tumor.
If a tumor nodule was identified, it could be confirmed with a targeted, MRI-guided biopsy. The cancer detection rate for MRI directed biopsy is around 80 percent compared to 45 percent at time of first TRUS biopsy.
During MRI-guided biopsy, fewer needles are also inserted into the prostate gland. This helps to reduce the number of potential complications.
Prostate MRI provides several important data points about a prostate cancer tumor(s). It can:
- Measure the extent of tumor volume.
- Identify the tumor’s location or locations in the gland.
- Estimate how aggressive the tumor is, which is critical to planning accurate biopsy guidance.
- Reveal staging information.
- Determine whether the tumor has spread beyond the prostate gland.
- Roughly 225,000 men will be diagnosed with prostate cancer this year – 28,000 men will die of prostate cancer.
- There are more than 1 million prostate biopsies being performed each year.
How can we improve upon prostate MRI and TRUS biopsy?
There are few centers experienced in performing and interpreting prostate MRI – many of these do not have high field high field 3T magnets to provide optimal imaging quality that helps to improves accuracy. A new procedure is now available for men to improve our ability to more accurately detect prostate cancer with fewer needles and higher yields – MRI-TRUS fusion.
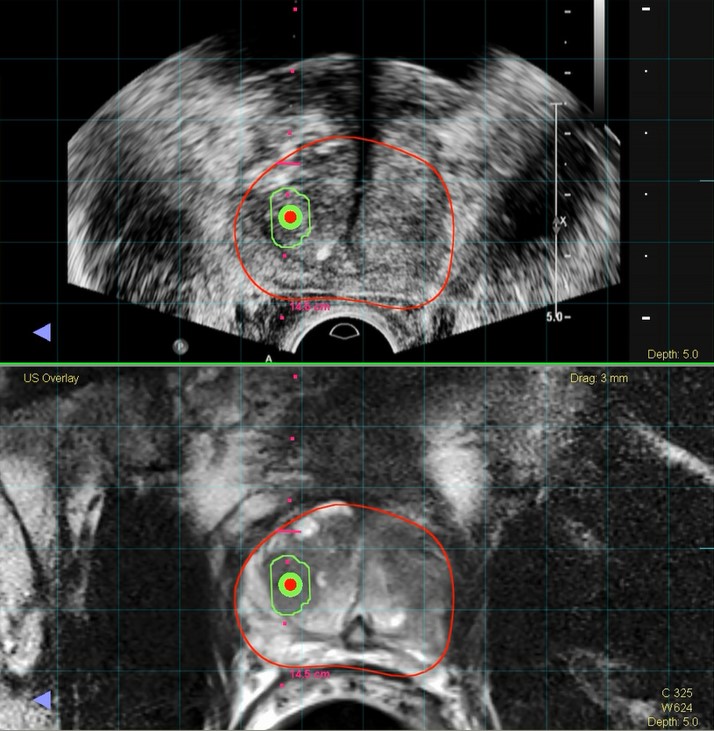
An in-bore, MRI-guided prostate biopsy is an expensive and time-consuming procedure that can last longer than one hour. Urologists familiar with standard TRUS can perform a biopsy in 10 to 15 minutes at relatively low cost. MRI-TRUS fusion was developed to combine the benefits of MRI-guided biopsy with the less time-consuming, more cost-effective benefits of TRUS.
In MRI-TRUS fusion biopsies, functional data and anatomic detail provided by multiparametric prostate MRI is electronically delivered to special fusion ultrasound machines. This allows urologists to use the detail provided during prostate MRI to guide live, real-time ultrasound scanning.